by Libby James
When John Spencer joined a team of microbiologists and immunologists at Colorado State University in 1995, he had been intrigued by leprosy and the challenges presented by the disease for more than a decade. While pursuing a degree in microbiology at the University of Hawaii in 1984, he was one of only a few people permitted to visit Kalaupapa, the leper colony on the tiny island of Molokai. Over the course of a century, 8,000 people infected with the disease had been banished to this lonely spot bordered by the sea and a series of cliffs making escape impossible.
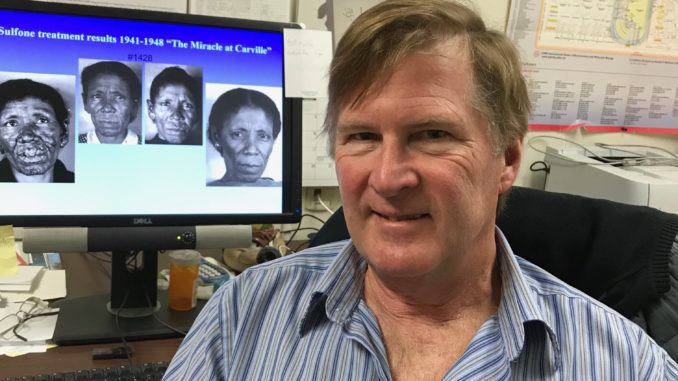
Spencer went on to earn graduate degrees and do cancer research in Philadelphia. After completing a postdoc focused on immunology at National Jewish Hospital in Denver, he came to CSU to work on tuberculosis and leprosy. Today he works with a group of 23 principal investigators, part of the largest group of its kind in the U.S.
After 23 years, he remains as passionate as ever about his work, especially his efforts to contribute to the creation of a simple test to determine a person’s risk for developing leprosy. He hopes that eventually, they will be able to develop a preventive vaccine. Discovering a person’s risk for developing leprosy before there are any visible symptoms would go a long way toward making prevention simple and effective.
The most ancient disease known to man, years ago leprosy instilled such fear among people that sufferers were forced into isolation and no longer considered human. They were given a number and a new name and permanently separated from their families and communities.
Understandably, diagnosis caused extreme anxiety. Patients believed they were cursed and worried about how their families would deal with the stigma connected with the disease. There were common misconceptions about how leprosy could be passed on. It is not extremely contagious. It can be spread by coughing and sneezing but more often is contracted by a long-term association with an affected individual. Also, studies show that there may be a genetic component. “However,” Spencer notes, “90 percent of the population is naturally immune to the disease and therefore will never contract it.”
Leprosy develops so slowly that it takes from three to seven years to become active. Over time it can cause skin lesions, paralysis, blindness, nerve damage and disfigurement. Today, treatment with a series of antibiotics is extremely effective and has tempered the frightening aspects of the disease. After only two weeks of treatment, patients are no longer contagious.
There are only a few remnants of the original populations still living at Kalaupapa and at the Carville leper colony in Louisiana. Sufferers and former sufferers are no longer forced to remain in isolation. They are free to return to society, but some have lived in the colonies for so long that they have become the only home the residents know. They have married and had children and have elected to stay.
Carville was a more humane environment than Kalaupapa. The emphasis was on care rather than imprisonment and it was in Carville in 1940 that Dr. Isadora Dyer developed the sulfone drug therapy that became a cure. The well-known book, “Miracle at Carville,” tells the story.
Spencer spends a part of each year in Brazil, a country that has more new cases of leprosy per capita than any place in the world. Other countries with high incidences of the disease are India, Indonesia, Southeast Asia and the Pacific Islands. There are only 200 new cases each year in the U.S.
In Brazil, Spencer works with local researchers and doctors, visits schools and helps educate citizens about the risks of getting the disease. Anyone diagnosed is given free treatment.
In the last few decades, a strange turnabout phenomenon has emerged. Nine band armadillos, in the past injected with leprosy in the course of research, are now transmitting the disease to humans. In the area in northern Brazil where Spencer works, people frequently interact with armadillos, as pets and as a source of food. Part of Spencer’s work is educating the public on precautions to take when coming into contact with armadillos.
Seventy-five percent of the cases of leprosy diagnosed each year in the U.S. are found in people who have come from other countries. The remaining cases are largely from areas where armadillos are common in the U.S.
Spencer has authored several articles on his work and has made connections with researchers in other countries as they work together to wipe out this once-dreaded disease.
Support Northern Colorado Journalism
Show your support for North Forty News by helping us produce more content. It's a kind and simple gesture that will help us continue to bring more content to you.
BONUS - Donors get a link in their receipt to sign up for our once-per-week instant text messaging alert. Get your e-copy of North Forty News the moment it is released!
Click to Donate